Research has shown that the COVID-19 pandemic has magnified the prevalence of eating disorders across all demographics. Isolation, fear, and lack of control have created what many refer to as the “perfect storm” for eating disorder behaviors to brew.
With research comes a greater understanding of risk factors and more effective treatments.
Increased hospitalizations in children and adolescents for eating disorders
During the pandemic, 15 children’s hospitals reported that admissions for eating disorders doubled, on average.
A Canadian study found that acute care visits for pediatric eating disorders increased significantly after the onset of pandemic and remained well above expected levels during the first 10 months of the pandemic.
These findings are in line with what Walden has seen with the doubling of calls to our admissions department since the beginning of the pandemic.
The impact of the pandemic will undoubtedly have lasting effects on the mental health of many people.
Virtual eating disorder therapy is a viable alternative to in-person therapy
Another pandemic-inspired study showed virtual therapy conducted using internet-based videoconferencing to be a viable alternative to in-person therapy for a variety of mental-health problems including eating disorder treatment.
According to the study, participants showed similar improvements on eating symptoms, levels of weight gain (in individuals in whom gain was indicated), and satisfaction with services.
At Walden, we found that offering virtual therapy meant greater access to patients and families who may have otherwise not been able to attend in-person therapy for a variety of reasons including scheduling, lack of transportation, and other mental health challenges.
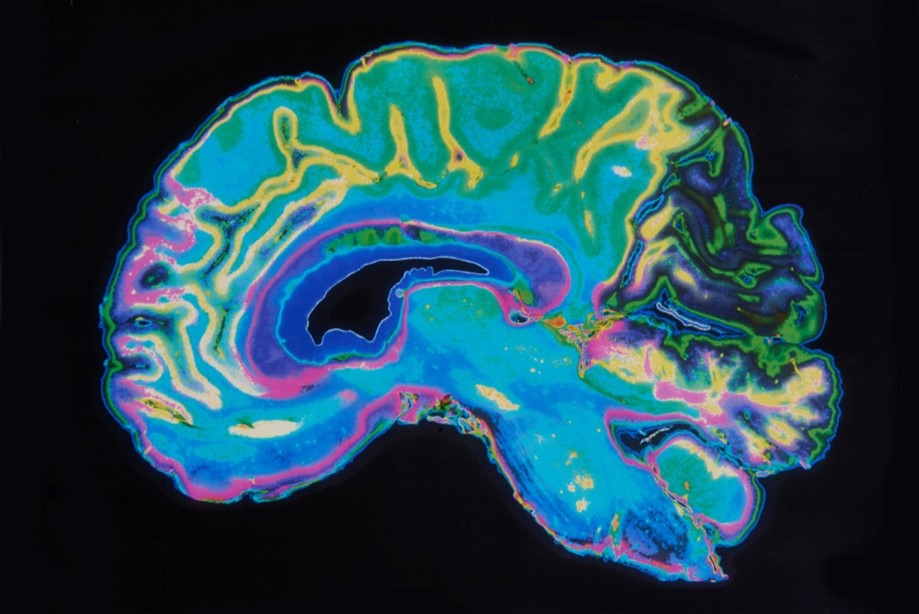
Anorexia can lead to shrinking of brain structure
A recent study that involved research teams around the world analyzed the impact a lack of sufficient nutrition can have on the brain.
The study looked at 1,648 female brain scans (685 with anorexia nervosa) collected from 22 different locations. The researchers found decreases in cortical thickness, subcortical volumes, and cortical surface area in people with anorexia. Essentially, the brain shrinks down under anorexia.
There was some positive news, however. The brain scans showed that anorexia treatment could possibly reverse some of these changes in the brain structure, which reinforces the importance of seeking early treatment.
“This is a good sign, because it indicates that these changes might not be permanent. With the right treatment, the brain might be able to bounce back,” says psychologist Esther Walton, from the University of Bath in the UK.
Benefit of athlete-specific eating disorder treatment
Walden believes in meeting people where they are on their recovery journey with individualized care. Based on recent research, athlete-specific eating disorder treatment has positive and measurable effects of decreasing eating disorder behavioral risks, eating pathology, and increasing eating competence in this segment of the population.
When asked about participating in Walden’s GOALS Program for athletes, clients felt that the program was customized and addressed their unique needs, which helped to glean more meaningful and desired treatment outcomes for the athletes.
We know that research like this advances our collective knowledge of the complexities around eating disorders and related mental health conditions. It is our hope that it furthers our goal to provide more effective and accessible treatment options for those in need.
If you are concerned that you, or a loved one, may have an eating disorder, please reach out by completing the form on this page or email us at intake_coordinators@waldenbehavioralcare.com.